Myocardial infarction
| Myocardial infarction | |
|---|---|
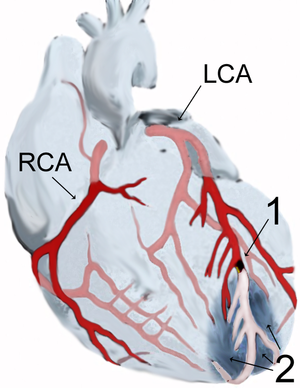
Diagram of a myocardial infarction (2) of the
anterior wall of the heart after blockage (1) of a branch of the
left coronary artery (LCA). In the diagram, RCA is the
right coronary artery.
|
|
| Classification and external resources | |
| Specialty | Cardiology |
| ICD-10 | I21-I22 |
| ICD-9-CM | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
| Patient UK | Myocardial infarction |
| MeSH | D009203 |
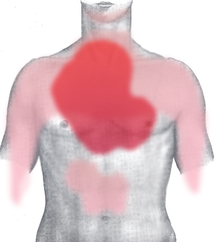
Myocardial infarction (MI) or acute myocardial infarction (AMI), commonly known as a heart attack, occurs when blood flow stops to a part of the heart causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Often it is in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, or feeling tired.[1] About 30% of people have atypical symptoms,[2] with women more likely than men to present atypically.[3] Among those over 75 years old, about 5% have had an MI with little or no history of symptoms.[4] An MI may cause heart failure, an irregular heartbeat, or cardiac arrest.[5][6]
Most MIs occur due to coronary artery disease.[5] Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol intake, among others.[7][8] The mechanism of an MI often involves the complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque.[5] MIs are less commonly caused by coronary artery spasms, which may be due to cocaine, significant emotional stress, and extreme cold, among others.[9][10] A number of tests are useful to help with diagnosis, including electrocardiograms (ECGs), blood tests, and coronary angiography.[11] An ECG may confirm an ST elevation MI if ST elevation is present.[2] Commonly used blood tests include troponin and less often creatine kinase MB.[11]
Aspirin is an appropriate immediate treatment for a suspected MI.[12] Nitroglycerin or opioids may be used to help with chest pain; however, they do not improve overall outcomes.[2][12] Supplemental oxygen should be used in those with low oxygen levels or shortness of breath.[12] In ST elevation MIs treatments which attempt to restore blood flow to the heart are typically recommended and include angioplasty, where the arteries are pushed open, or thrombolysis, where the blockage is removed using medications.[2] People who have a non-ST elevation myocardial infarction (NSTEMI) are often managed with the blood thinner heparin, with the additional use of angioplasty in those at high risk.[12] In people with blockages of multiple coronary arteries and diabetes, bypass surgery (CABG) may be recommended rather than angioplasty.[13] After an MI, lifestyle modifications, along with long term treatment with aspirin, beta blockers, and statins, are typically recommended.[2]
Worldwide, about 8.6 million myocardial infarctions occurred in 2013.[14] More than 3 million people had an ST elevation MI and more than 4 million had an NSTEMI.[15] STEMIs occur about twice as often in men as women.[16] About one million people have an MI each year in the United States.[5] In the developed world the risk of death in those who have had an STEMI is about 10%.[2] Rates of MI for a given age have decreased globally between 1990 and 2010.[17]
Signs and symptoms[edit]
The onset of symptoms in myocardial infarction (MI) is usually gradual, over several minutes, and rarely instantaneous.[18] Chest pain is the most common symptom of acute MI and is often described as a sensation of tightness, pressure, or squeezing. Chest pain due to ischemia (a lack of blood and hence oxygen supply) of the heart muscle is termed angina pectoris. Pain radiates most often to the left arm, but may also radiate to the lower jaw, neck, right arm, back, and upper abdomen,[19] where it may mimic heartburn. Levine's sign, in which a person localizes the chest pain by clenching their fists over their sternum, has classically been thought to be predictive of cardiac chest pain, although a prospective observational study showed it had a poor positive predictive value.[20]
Shortness of breath occurs when the damage to the heart limits the output of the left ventricle, causing left ventricular failure and consequent pulmonary edema. Other symptoms include diaphoresis (an excessive form of sweating),[21] weakness, light-headedness, nausea, vomiting, and palpitations. These symptoms are likely induced by a massive surge of catecholamines from the sympathetic nervous system,[22] which occurs in response to pain and the blood flow abnormalities that result from dysfunction of the heart muscle. Loss of consciousness (due to inadequate blood flow to the brain and cardiogenic shock) and sudden death (frequently due to the development of ventricular fibrillation) can occur in MIs.[19]
Atypical symptoms are more frequently reported by women, the elderly, and those with diabetes when compared to their male and younger counterparts.[23][24] Women also report more numerous symptoms compared with men (2.6 on average vs. 1.8 symptoms in men).[23] The most common symptoms of MI in women include dyspnea, weakness, and fatigue. Fatigue, sleep disturbances, and dyspnea have been reported as frequently occurring symptoms that may manifest as long as one month before the actual clinically manifested ischemic event. In women, chest pain may be less predictive of coronary ischemia than in men.[25] Women may also experience back or jaw pain during an episode.[26]
At least one quarter of all MIs happen without chest pain or other symptoms.[4] These cases can be discovered later on electrocardiograms, using blood enzyme tests, or at autopsy without a prior history of related complaints. Estimates of the prevalence of silent MIs vary between 22 and 64%.[4] A silent course is more common in the elderly,[4] in people with diabetes mellitus[27] and after heart transplantation, probably because the donor heart is not fully innervated by the nervous system of the recipient.[28] In people with diabetes, differences in pain threshold, autonomic neuropathy, and psychological factors have been cited as possible explanations for the lack of symptoms.[27]
Any group of symptoms compatible with a sudden interruption of the blood flow to the heart, which includes STEMI, NSTEMI or unstable angina, are called an acute coronary syndrome.[29]
Causes[edit]
Many of the risk factors for myocardial infarction are modifiable and thus many cases may be preventable.
Lifestyle[edit]
Smoking appears to be the cause of about 36% and obesity the cause of 20% of coronary artery disease.[30] Lack of exercise has been linked to 7–12% of cases.[30][31] Less common causes include stress-related causes such as job stress, which accounts for about 3% of cases,[30] and chronic high stress levels.[32]
Tobacco smoking (including secondhand smoke)[33] and short-term exposure to air pollution such as carbon monoxide, nitrogen dioxide, and sulfur dioxide (but not ozone) have been associated with MI.[34] Other factors that increase the risk of MI and are associated with worse outcomes after an MI include lack of physical activity[35] and psychosocial factors including low socioeconomic status, social isolation, and negative emotions. Shift work is also associated with a higher risk of MI.[36] Acute and prolonged intake of high quantities of alcoholic drinks (3-4 or more) increase the risk of a heart attack.[37]
The evidence for saturated fat is unclear. Some state there is evidence of benefit from reducing saturated fat,[38] specifically a benefit from eating polyunsaturated fat instead of saturated fat.[39] While others state there is little evidence that reducing dietary saturated fat or increasing polyunsaturated fat intake affects heart attack risk.[40][41] Dietary cholesterol does not appear to have a significant effect on blood cholesterol and thus recommendations about its consumption may not be needed.[42] Trans fats do appear to increase risk.[40]
Disease[edit]
Diabetes mellitus (type 1 or 2),[43] high blood pressure,[33] dyslipidemia/high levels of blood cholesterol (abnormal levels of lipoproteins in the blood), particularly high low-density lipoprotein, low high-density lipoprotein, high triglycerides,[33] endometriosis in women under the age of 40[44] and obesity[45] (defined by a body mass index of more than 30 kg/m², or alternatively by waist circumference or waist-hip ratio) have all been linked to MI.
A number of acute and chronic infections including Chlamydophila pneumoniae, influenza, Helicobacter pylori, and Porphyromonas gingivalis among others have been linked to atherosclerosis and myocardial infarction.[46] As of 2013, there is no evidence of benefit from antibiotics or vaccination, however, calling the association into question.[46][47] Myocardial infarction can also occur as a late consequence of Kawasaki disease.[48]
Genetic[edit]
Genome-wide association studies have found 27 genetic variants that are associated with an increased risk of myocardial infarction.[49] Strongest association of MI has been found with the 9p21 genomic locus, which contains genes CDKN2A & 2B, although the single nucleotide polymorphisms that are implicated are within a non-coding region.[49] The majority of these variants are in regions that have not been previously implicated in coronary artery disease. The following genes have an association with MI: PCSK9, SORT1, MIA3, WDR12, MRAS, PHACTR1, LPA, TCF21, MTHFDSL, ZC3HC1, CDKN2A, 2B, ABO, PDGF0, APOA5, MNF1ASM283, COL4A1, HHIPC1, SMAD3, ADAMTS7, RAS1, SMG6, SNF8, LDLR, SLC5A3, MRPS6, KCNE2.[49]
Other[edit]
At any given age, men are more at risk than women, particularly before menopause,[50] but because in general women live longer than men, ischemic heart disease causes slightly more total deaths in women.[35] Family history of ischemic heart disease or MI, particularly if one has a first-degree relative (father, brother, mother, sister) who suffered a 'premature' myocardial infarction (defined as occurring at or younger than age 55 years (men) or 65 (women)).[35]
Women who use combined oral contraceptive pills have a modestly increased risk of myocardial infarction, especially in the presence of other risk factors, such as smoking.[51] Heart attacks appear to occur more commonly in the morning hours, especially between 6AM and noon.[52] Evidence suggests that heart attacks are at least three times more likely to occur in the morning than in the late evening.[53] Old age increases risk of a heart attack.[35]
Pathophysiology[edit]

Acute myocardial infarction refers to two subtypes of acute coronary syndrome, namely non-ST-elevated and ST-elevated MIs, which are most frequently (but not always) a manifestation of coronary artery disease.[54] The most common triggering event is the disruption of an atherosclerotic plaque in an epicardial coronary artery, which leads to a clotting cascade, sometimes resulting in total occlusion of the artery.[55][56] Atherosclerosis is the gradual buildup of cholesterol and fibrous tissue in plaques in the wall of arteries (in this case, the coronary arteries), typically over decades.[57] Bloodstream column irregularities visible on angiography reflect artery lumen narrowing as a result of decades of advancing atherosclerosis.[58] Plaques can become unstable, rupture, and additionally promote the formation of a blood clot that occludes the artery; this can occur in minutes. When a severe enough plaque rupture occurs in the coronary arteries, it leads to MI (necrosis of downstream myocardium).[55][56] It is estimated that one billion cardiac cells are lost in a typical MI.[59]
If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the occluded coronary artery die (chiefly through necrosis) and do not grow back. A collagen scar forms in their place. Recent studies indicate that another form of cell death, apoptosis, also plays a role in the process of tissue damage following an MI.[60] As a result, the person's heart will be permanently damaged. This myocardial scarring also puts the person at risk for potentially life-threatening abnormal heart rhythms (arrhythmias), and may result in the formation of a ventricular aneurysm that can rupture with catastrophic consequences.
Injured heart tissue conducts electrical impulses more slowly than normal heart tissue. The difference in conduction velocity between injured and uninjured tissue can trigger re-entry or a feedback loop that is believed to be the cause of many lethal arrhythmias. The most serious of these arrhythmias is ventricular fibrillation (V-Fib/VF), an extremely fast and chaotic heart rhythm that is the leading cause of sudden cardiac death. Another life-threatening arrhythmia is ventricular tachycardia (V-tach/VT), which can cause sudden cardiac death. However, VT usually results in rapid heart rates that prevent the heart from pumping blood effectively. Cardiac output and blood pressure may fall to dangerous levels, which can lead to further coronary ischemia and extension of the infarct.
The cardiac defibrillator device was specifically designed to terminate these potentially fatal arrhythmias. The device works by delivering an electrical shock to the person to depolarize a critical mass of the heart muscle, in effect "rebooting" the heart. This therapy is time-dependent, and the odds of successful defibrillation decline rapidly after the onset of cardiopulmonary arrest.
Myocardial infarction in the setting of plaque results from underlying atherosclerosis.[19] Inflammation is known to be an important step in the process of atherosclerotic plaque formation.[61] C-reactive protein (CRP) is a sensitive but nonspecific marker for inflammation. Elevated CRP blood levels, especially measured with high-sensitivity assays, can predict the risk of MI, as well as stroke and development of diabetes.[61] Moreover, some drugs for MI might also reduce CRP levels.[61] The use of high-sensitivity CRP assays as a means of screening the general population is advised against, but it may be used optionally at the physician's discretion in those who already present with other risk factors or known coronary artery disease.[62] Whether CRP plays a direct role in atherosclerosis remains uncertain.[61]
Calcium deposition as calcification is another part of atherosclerotic plaque formation. Calcium deposits in the coronary arteries can be detected with CT scans. Several studies have shown that coronary calcium can provide predictive information beyond that of classical risk factors.[63][64][65]
Hyperhomocysteinemia (high blood levels of the amino acid homocysteine) in homocysteinuria is associated with premature atherosclerosis;[66] whether elevated homocysteine in the normal range is causal is controversial.[67]
Pathological types[edit]
The two main types of acute myocardial infarction, based on pathology, are:
- Transmural AMI is associated with atherosclerosis involving a major coronary artery. It can be subclassified into anterior, posterior, inferior, lateral, or septal. Transmural infarcts extend through the whole thickness of the heart muscle and are usually a result of complete occlusion of the area's blood supply.[68] In addition, on ECG, ST elevation and Q waves are seen.
- Subendocardial AMI involves a small area in the subendocardial wall of the left ventricle, ventricular septum, or papillary muscles. The subendocardial area is particularly susceptible to ischemia.[68] In addition, ST depression may be seen on ECG in addition to T wave changes.
Diagnosis[edit]

A cardiac troponin rise accompanied by either typical symptoms, pathological Q waves, ST elevation or depression, or coronary intervention is diagnostic of MI.[69]
WHO criteria[70] formulated in 1979 have classically been used to diagnose MI; a patient is diagnosed with MI if two (probable) or three (definite) of the following criteria are satisfied:
- Clinical history of ischemic-type chest pain lasting for more than 20 minutes
- Changes in serial ECG tracings
- Rise and fall of serum cardiac biomarkers
At autopsy, a pathologist can diagnose an MI based on anatomopathological findings.
Classification[edit]
Myocardial infarctions are generally classified into ST elevation MI (STEMI) and non-ST elevation MI (NSTEMI).[54] A STEMI is the combination of symptoms related to poor oxygenation of the heart with elevation of the ST segments on the electrocardiogram followed by an increase in proteins in the blood related to heart muscle's death.[16] They make up about 25 to 40 percent of cases.[16]
The phrase "heart attack" is often used non-specifically to refer to a myocardial infarction and to sudden cardiac death. An MI is different from—but can cause—cardiac arrest, where the heart is not contracting at all or so poorly that all vital organs cease to function. It is also distinct from heart failure, in which the pumping action of the heart is impaired. However, an MI may lead to heart failure.[19]
A 2007 consensus document classifies MI into five main types:[71]
- Type 1 – spontaneous MI related to ischemia due to a primary coronary event such as plaque erosion and/or rupture, fissuring, or dissection
- Type 2 – MI secondary to ischemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anemia, arrhythmias, hypertension, or hypotension
- Type 3 – sudden unexpected cardiac death, including cardiac arrest, often with symptoms suggestive of myocardial ischemia, accompanied by new ST elevation, or new left bundle branch block (LBBB), or evidence of fresh thrombus in a coronary artery by angiography and/or at autopsy, but death occurring before blood samples could be obtained, or at a time before the appearance of cardiac biomarkers in the blood
- Type 4 – associated with
coronary angioplasty or stents:
- Type 4a – MI associated with percutaneous coronary intervention (PCI)
- Type 4b – MI associated with stent thrombosis as documented by angiography or at autopsy
- Type 5 – MI associated with CABG
The terms Q wave and non-Q wave MI were previously used to indicate STEMI and non-STEMI respectively.[72]
Electrocardiogram[edit]
For a person to qualify as having a STEMI, in addition to reported angina, the ECG must show new ST elevation in two or more adjacent ECG leads.[16] This must be greater than 2 mm (0.2 mV) for males and greater than 1.5 mm (0.15 mV) in females if in leads V2 and V3 or greater than 1 mm (0.1 mV) if it is in other ECG leads.[16] A left bundle branch block that is believed to be new used to be considered the same as ST elevation; however, this is no longer the case.[16] In early STEMIs there may just be peaked T waves with ST elevation developing later.[16]
Cardiac biomarkers[edit]
While there are a number of different biomarkers, troponins are considered to be the best[16] and reliance on older tests (such as CK-MB) or myoglobin is discouraged.[73] This is not the case in the setting of peri-procedural MI where use of troponin and CK-MB assays are considered useful.[74] Copeptin may be useful to rule out MI rapidly when used along with troponin.[75]
Imaging[edit]
A chest radiograph and routine blood tests may indicate complications or precipitating causes, and are often performed upon arrival to an emergency department.
In stable patients whose symptoms have resolved by the time of evaluation, technetium (99mTc) sestamibi (i.e. a "MIBI scan") or thallium-201 chloride can be used in nuclear medicine to visualize areas of reduced blood flow in conjunction with physiological or pharmacological stress. Thallium may also be used to determine viability of tissue, distinguishing whether nonfunctional myocardium is actually dead or merely in a state of hibernation or of being stunned.[76] Medical societies and professional guidelines recommend that the physician confirm a person is at high risk for myocardial infarction before conducting imaging tests to make a diagnosis.[77][78] Patients who have a normal ECG and who are able to exercise, for example, do not merit routine imaging.[78] Imaging tests such as stress radionuclide myocardial perfusion imaging or stress echocardiography can confirm a diagnosis when a patient's history, physical exam, ECG, and cardiac biomarkers suggest the likelihood of a problem.[78]
Differential diagnosis[edit]
The differential diagnosis for MI includes other catastrophic causes of chest pain, such as pulmonary embolism, aortic dissection, esophageal rupture, tension pneumothorax, or pericardial effusion causing cardiac tamponade. Other noncatastrophic differentials include gastroesophageal reflux and Tietze's syndrome.[79]
Prevention[edit]
Myocardial infarction and other related cardiovascular diseases can be prevented to a large extent by a number of lifestyle changes and medical treatments.
Lifestyle[edit]
Recommendations include increasing the intake of wholegrain starch, reducing sugar intake (particularly of refined sugar), consuming five portions of fruit and vegetables daily, consuming two or more portions of fish per week, and consuming 4–5 portions of unsalted nuts, seeds, or legumes per week.[80] The dietary pattern with the greatest support is the Mediterranean diet.[81] Vitamins and mineral supplements are of no proven benefit,[82] and neither are plant stanols or sterols.[80]
There is some controversy surrounding the effect of dietary fat on the development of cardiovascular disease. People are often advised to keep a diet where less than 30% of the energy intake derives from fat, a diet that contains less than 7% of the energy intake in the form of saturated fat, and a diet that contains less than 300 mg/day of cholesterol.[80] Replacing saturated with mono- polyunsaturated fat is also recommended,[80] as the consumption of polyunsaturated fat instead of saturated fat may decrease coronary heart disease.[83] Olive oil, rapeseed oil and related products are to be used instead of saturated fat.[80]
Physical activity can reduce the risk of cardiovascular disease, and people at risk are advised to engage in 150 minutes of moderate or 75 minutes of vigorous intensity aerobic exercise a week.[80] Keeping a healthy weight, drinking alcohol within the recommended limits, and quitting smoking are measures that also appear to reduce the risk of cardiovascular disease.[80]
On a population level, public health measures may be used to reduce unhealthy diets (excessive salt, saturated fat and trans fat) including food labeling and marketing requirements as well as requirements for catering and restaurants, and stimulating physical activity. This may be part of regional cardiovascular disease prevention programs, or through the health impact assessment of regional and local plans and policies.[84]
Medication[edit]
Aspirin has been studied extensively in people considered at increased risk of myocardial infarction. Based on numerous studies in different groups (e.g. people with or without diabetes), there does not appear to be a benefit strong enough to outweigh the risk of excessive bleeding.[85][86] Nevertheless, many clinical practice guidelines continue to recommend aspirin for primary prevention,[87] and some researchers feel that those with very high cardiovascular risk but low risk of bleeding should continue to receive aspirin.[88]
Cholesterol-lowering drugs from the statin class may be used in those at an elevated risk of cardiovascular disease; this can be calculated with validated risk prediction tools such as QRISK2.[80]
Long term hormone replacement therapy when started around the time of menopause may decrease heart disease.[89][90]
Following a heart attack, nitrates, when taken for two days, and ACE-inhibitors decrease the risk of death.[91]
Management[edit]
An MI requires immediate medical attention. Treatment attempts to save as much viable heart muscle as possible and to prevent further complications, hence the phrase "time is heart muscle".[92] Aspirin and nitroglycerin may be administered. Nitroglycerin (administered under the tongue or intravenously) may be administered to improve the blood supply to the heart.[73] Morphine may be used if nitroglycerin is not effective.[73] Other analgesics such as nitrous oxide are of unknown benefit.[93]
In the past, high flow oxygen was recommended for everyone with possible myocardial infarction.[73] More recently, routine use was found to lead to increased mortality and infarct size.[94][95] Therefore, oxygen is currently only used if oxygen levels are found to be low or someone is in respiratory distress.[73] A 2015 meta-analysis concluded that the use of an intra-aortic balloon pump during an acute MI with or without cardiogenic shock does not reduce mortality.[96]
STEMI[edit]
The main treatment for MI with ECG evidence of ST elevation (STEMI) include thrombolysis and percutaneous coronary intervention.[97] Primary percutaneous coronary intervention (PCI) is the treatment of choice for STEMI if it can be performed in a timely manner.[97][98] If PCI cannot be performed within 90 to 120 minutes then thrombolysis, preferably within 30 minutes of arrival to hospital, is recommended.[98][99][100] If a person has had symptoms for 12 to 24 hours evidence for thrombolysis is less and if they have had symptoms for more than 24 hours it is not recommended.[101]
Thrombolysis involves the administration of medication that activates the enzymes that normally destroy blood clots. Thrombolysis agents include streptokinase, reteplase, alteplase, and tenecteplase. If no contraindications are present (such as a high risk of bleeding), thrombolysis can be given in the pre-hospital or in-hospital setting. When given to people suspected of having a STEMI within 6 hours of the onset of symptoms, thrombolytic drugs save the life of 1 in 43 who received them. The risks were major bleeding (1 in 143) and brain bleeding (1 in 250).[102][103] It is unclear whether pre-hospital thrombolysis reduces death in people with STEMI compared to in-hospital thrombolysis.[104] Pre-hospital thrombolysis reduces time to thrombolytic treatment, based on studies conducted in higher income countries.[104]
If despite thrombolysis there is significant cardiogenic shock, continued severe chest pain, or less than a 50% improvement in ST elevation on the ECG recording after 90 minutes, then rescue PCI is indicated emergently.[99][105] After PCI, people are generally placed on dual antiplatelet therapy for at least a year (which is generally aspirin and clopidogrel).[16][97][106]
When beta blocker medication are given within the first 24–72 hours of a major heart attack (“STEMI”) no lives are saved. However, 1 in 200 people were prevented from a repeat heart attack, and another 1 in 200 from having an abnormal heart rhythm. Additionally, for 1 in 91 the drug causes a temporary poor ability of the heart to pump blood.[107]
Those who have had cardiac arrest may benefit from targeted temperature management with evaluation for implementation of hypothermia protocols. Furthermore, those with cardiac arrest, and ST elevation at any time, should usually have angiography.[108]
NSTEMI[edit]
In the absence of ST elevation, diagnosis of MI is based on a blood test for biomarkers (usually troponin). This can take 3–6 hours after the onset of symptoms to become positive. The scenario is referred to as "non-ST elevation acute coronary syndrome" (NSTEACS). In the meantime, the calculated risk of further cardiovascular events (e.g. using the GRACE score) and the presence of other ECG changes and clinical features determines ongoing management.[73][77]
People with an acute coronary syndrome where no ST elevation is demonstrated (non-ST elevation ACS or NSTEACS) are treated with aspirin.[73][77] Clopidogrel is added in many cases, particularly if the risk of cardiovascular events is felt to be high and early PCI is being considered.[73][77] Depending on whether early PCI is planned, a factor Xa inhibitor or a potentiator of antithrombin (fondaparinux or low molecular weight heparin respectively) may be added.[77] In very high-risk scenarios, inhibitors of the platelet glycoprotein αIIbβ3a receptor such as eptifibatide or tirofiban may be used.[73][77]
Heparins in those who have had an NSTEMI or unstable angina do not change the risk of death.[109] They do decrease the risk of having a further myocardial infarction.[109]
As of 2011, P2Y12 inhibitors are recommended for 12 months following NSTEMI in Europe.[110] A 2014 review of P2Y12 inhibitors such as clopidogrel found they do not change the risk of death when given to people with a suspected NSTEMI prior to PCI. They do however increase the risk of bleeding and decrease the risk of further cardiovascular problems. The authors thus concluded that their routine use prior to PCI is of questionable value.[111]
Cardiac rehabilitation[edit]
Cardiac rehabilitation benefits many who have experienced myocardial infarction, even if there has been substantial heart damage and resultant left ventricular failure; ideally other medical conditions that could interfere with participation should be managed optimally. It should start soon after discharge from the hospital. The program may include lifestyle advice, exercise, social support, as well as recommendations about driving, flying, sport participation, stress management, and sexual intercourse.[112]
Secondary prevention[edit]
A number of lifestyle recommendations are available to those who have experienced myocardial infarction. This includes the adoption of a Mediterranean-type diet, maintaining alcohol intake within recommended limits, exercising to the point of mild breathlessness for 20–30 minutes every day, stopping smoking, and trying to achieve a healthy weight.[112] Exercise is both safe and effective even if people have had stents or heart failure.[113]
People are usually started on several long-term medications after an MI, with the aim of preventing further cardiovascular events such as MIs, congestive heart failure, or strokes.
- Aspirin as well as another antiplatelet agent such as clopidogrel or ticagrelor ("dual antiplatelet therapy" or DAPT) is continued for up to twelve months, followed by aspirin indefinitely.[112] If someone has another medical condition that requires anticoagulation (e.g. with warfarin) this may need to be adjusted based on risk of further cardiac events as well as bleeding risk.[112] In those who have had a stent, more than 12 months of clopidogrel plus aspirin does not affect the risk of death.[114]
- Beta blocker therapy such as metoprolol or carvedilol is recommended to be started within 24 hours, provided there is no acute heart failure or heart block.[16][73][112] The dose should be increased to the highest tolerated.[112] Contrary to what was long believed, the use of beta blockers does not appear to affect the risk of death, possibly because other treatments for MI have improved.[115] They should not be used in those who have recently taken cocaine.[116]
- ACE inhibitor therapy should be started when stable and continued indefinitely at the highest tolerated dose. Those who cannot tolerate ACE inhibitors may be treated with an angiotensin II receptor antagonist.[112]
- Statin therapy has been shown to reduce mortality and morbidity.[117] The protective effects of statins may be due to more than their LDL lowering effects. The general consensus is that statins have the ability to stabilize plaques and multiple other ("pleiotropic") effects that may prevent myocardial infarction in addition to their effects on blood lipids.[118]
- Aldosterone antagonists (spironolactone or eplerenone) may be used if there is evidence of left ventricular dysfunction after an MI, ideally after beginning treatment with an ACE inhibitor.[112]
- Previous studies suggested a benefit from omega-3 fatty acid supplementation but this has not been confirmed.[112]
Prognosis[edit]
The prognosis after MI varies greatly depending on a person's health, the extent of the heart damage, and the treatment given.
In those who have an STEMI in the United States, between 5 and 6 percent die before leaving the hospital and 7 to 18 percent die within a year.[16]
Using variables available in the emergency room, people with a higher risk of adverse outcome can be identified. One study found 0.4% of patients with a low-risk profile died after 90 days, whereas in high-risk people it was 21.1%.[119]
Some risk factors for death include age, hemodynamic parameters (such as heart failure, cardiac arrest on admission, systolic blood pressure, or Killip class of two or greater), ST-segment deviation, diabetes, serum creatinine, peripheral vascular disease, and elevation of cardiac markers.[119][120][121] Assessment of left ventricular ejection fraction may increase the predictive power.[122] Prognosis is worse if a mechanical complication such as papillary muscle or myocardial free wall rupture occurs.[123] Morbidity and mortality from myocardial infarction has improved over the years due to better treatment.[124]
Throughout hospital departments, practitioners use TIMI scores to assess mortality risk. There are TIMI (Thrombolysis in Myocardial Infarction) scores for unstable angina or NSTEMI[125] and STEMI,[126] both using routine patient data from history taking, medication use and lab results. Both scores have been found effective and reliable in multiple settings, including the emergency room.
Complications[edit]
Complications may occur immediately following the heart attack (in the acute phase), or may need time to develop (a chronic problem). Acute complications may include heart failure if the damaged heart is no longer able to pump blood adequately around the body; aneurysm of the left ventricle myocardium; ventricular septal rupture or free wall rupture; mitral regurgitation, in particular if the infarction causes dysfunction of the papillary muscle; Dressler's syndrome; and abnormal heart rhythms, such as ventricular fibrillation, ventricular tachycardia, atrial fibrillation, and heart block. Longer-term complications include heart failure, atrial fibrillation, and an increased risk of a second MI.
Epidemiology[edit]
Myocardial infarction is a common presentation of coronary artery disease. The World Health Organization estimated in 2004, that 12.2% of worldwide deaths were from ischemic heart disease;[127] with it being the leading cause of death in high- or middle-income countries and second only to lower respiratory infections in lower-income countries.[127] Worldwide, more than 3 million people have STEMIs and 4 million have NSTEMIs a year.[15] STEMIs occur about twice as often in men as women.[16]
Rates of death from ischemic heart disease (IHD) have slowed or declined in most high-income countries, although cardiovascular disease still accounted for one in three of all deaths in the USA in 2008.[128] For example, rates of death from cardiovascular disease have decreased almost a third between 2001 and 2011 in the United States.[129]
In contrast, IHD is becoming a more common cause of death in the developing world. For example, in India, IHD had become the leading cause of death by 2004, accounting for 1.46 million deaths (14% of total deaths) and deaths due to IHD were expected to double during 1985–2015.[130] Globally, disability adjusted life years (DALYs) lost to ischemic heart disease are predicted to account for 5.5% of total DALYs in 2030, making it the second-most-important cause of disability (after unipolar depressive disorder), as well as the leading cause of death by this date.[127]
Society and culture[edit]
In the United States, women who have had an MI are often treated with fewer medical interventions than men.[16] The word is from Latin: infarctus myocardii.
Economics[edit]
In 2011, AMI was one of the top five most expensive conditions seen during inpatient hospitalizations in the U.S., with an aggregate cost of about $11.5 billion for 612,000 hospital stays.[131]
Legal implications[edit]
At common law, in general, a myocardial infarction is a disease, but may sometimes be an injury. This can create coverage issues in the administration of no-fault insurance schemes such as workers' compensation. In general, a heart attack is not covered;[132] however, it may be a work-related injury if it results, for example, from unusual emotional stress or unusual exertion.[133] In addition, in some jurisdictions, heart attacks suffered by persons in particular occupations such as police officers may be classified as line-of-duty injuries by statute or policy. In some countries or states, a person having suffered from an MI may be prevented from participating in activity that puts other people's lives at risk, for example driving a car or flying an airplane.[134]